The Leading Value- Based Care Platform
LumerisPerformTM is the only end-to-end, technology enabled value-based care platform that improves patient care, lowers costs, and increases savings in total cost of care risk arrangements.

Comprehensive Value-Based Care Solutions to Support All Patient Lives
Care Quality & Access
Though directly responsible for only 2-6% of the total cost of care, primary care influences the vast majority of medical expense. Our Care Quality & Access solutions provide guideline-driven workflows and automated patient outreach for proactive screenings, tools to manage chronic diseases, pharmacy performance optimization, and tailored support to remove barriers that limit access to care.
Annually by PCP
*Representative Health System
*Due to complete & accurate documentation & coding
Documentation Accuracy
Our medical documentation solution set ensures risk and quality gaps are addressed promptly. We partner with providers to accurately identify all health conditions affecting a patient and systematically document any gaps in care. Our tech-powered solutions speed up the documentation process by providing real-time patient data for providers and office staff and comprehensively analyzing visit notes before submitting claims. Even for patients who have not seen a provider in a while, we support our partners with home visits to ensure precise health and documentation assessment.
Acute & Post-Acute CARE Orchestration
By leveraging our Acute & Post-Acute solution set, hospitalists, case managers, and therapists are able to employ strategies that maximize resource utilization and enhance care transitions. Technology-based processes, led by nurses, focus on reducing readmissions and maintaining communication for improved outcomes. We optimize home health and SNF services via strategic partnerships and minimize inappropriate use. High-performing post-acute networks are established through market performance assessment and the integration of strategic partnerships, analytics, and technology.
Length of Stay
*Representative Provider Group
*Highest risk 8-10% of the population
High-Risk Patient Management
At Lumeris, we’re revolutionizing how high-risk patients receive care using personalized, data-driven solutions. Leveraging Al and machine learning, our approach accurately identifies high-risk patients and offers comprehensive, prioritized support – at the patient’s home, virtually, and at the provider’s office. We also support partners with ED prevention and complex patient support capabilities.
Network Coordination
Our network coordination solutions intelligently connect patients with the most suitable in-network specialty providers and facility for optimum care outcomes. Leveraging our sophisticated algorithm, we factor in elements such as cost, outcome data, network status, insurance, and location amongst others. Our tech-powered solutions marry physician engagement services with best practice workflows, creating a seamless and automated coordination of care.
Out-of-Network
Utilization Claims
*Representative Provider Group
LumerisPerformTM is supported by our best in class technology for care orchestration and population health management
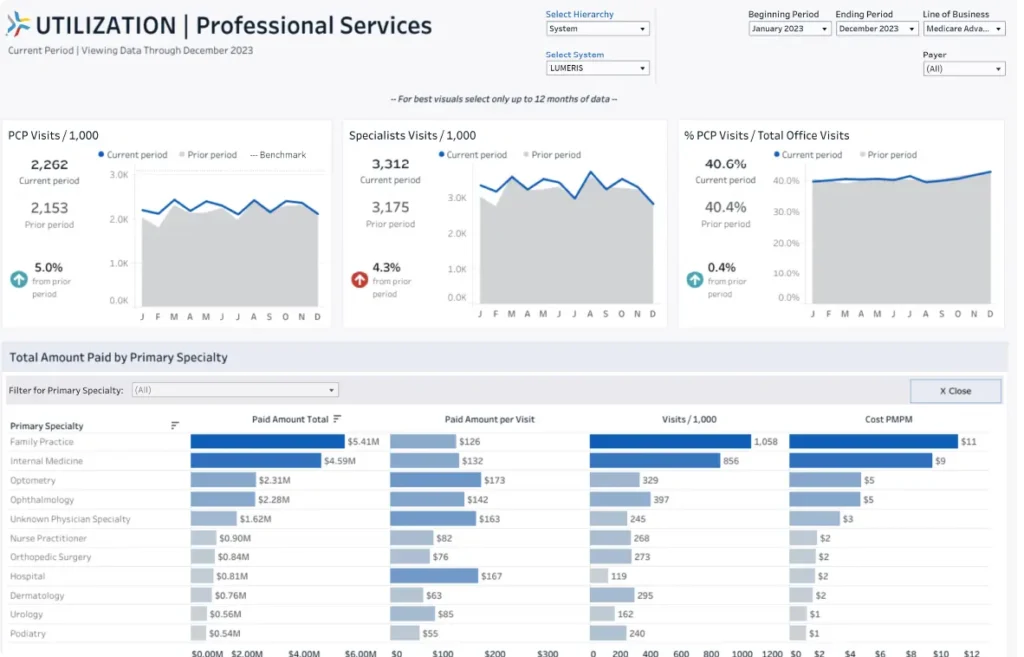

LumerisRealizeTM transforms large amounts of data into actionable reports and insights that identify care opportunities and trends by pulling and processing data from multiple data sources and leveraging intelligence capabilities and predictive analytics.
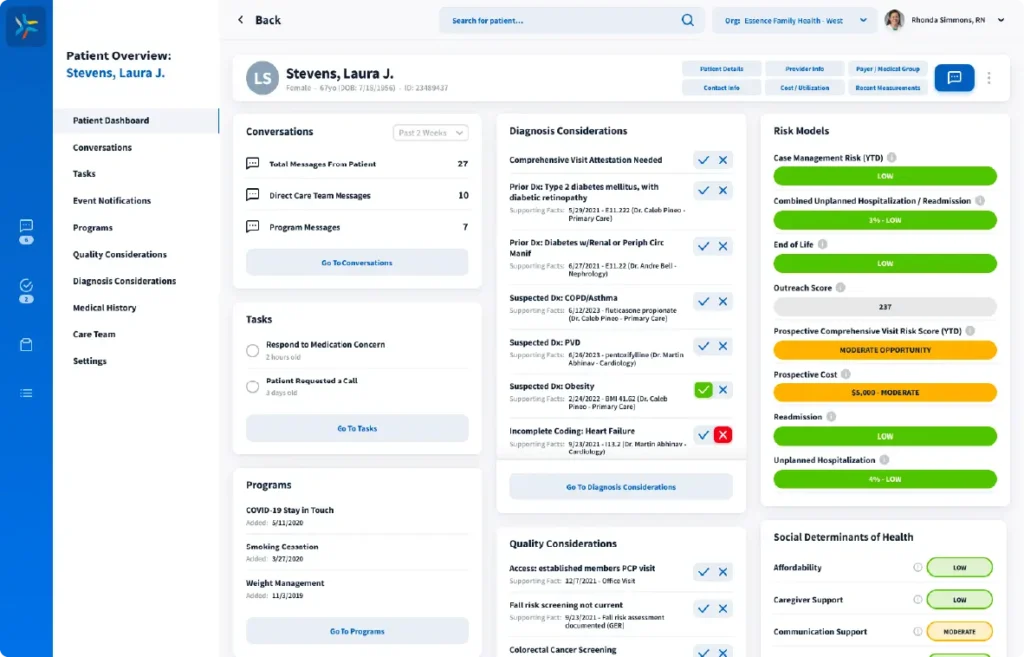

An Al-enabled platform built to engage physicians in proactive patient care, LumerisEngageTM operates between physicians and patients to promote real-time care interventions both at the point-of-care and at any time a patient wishes to engage.


