The future of healthcare isAI-powered & physician-empowering.
For more than 15 years, Lumeris has helped health systems and provider groups thrive in delivering high value patient care. Today, with Tom™—our AI-powered Primary Care as a Service platform—we deliver scalable, coordinated, and compassionate care that creates healthy systems, supports healthy people, and drives healthy outcomes.

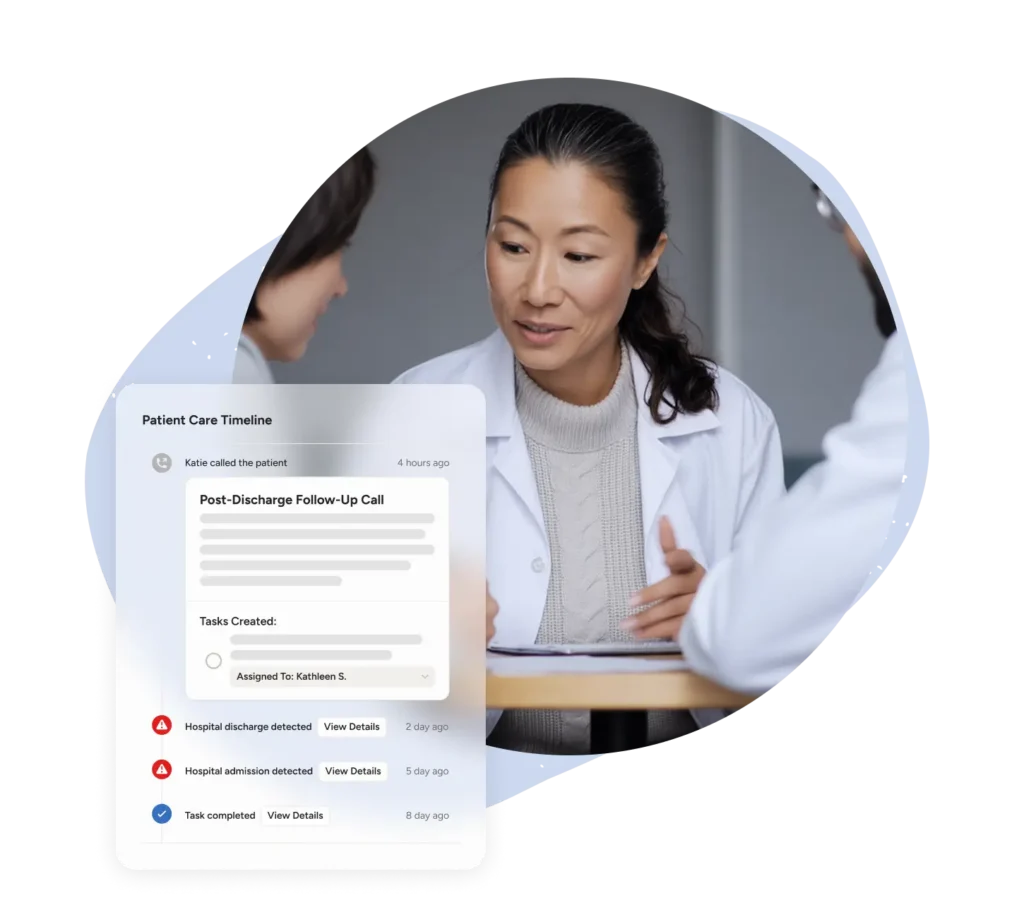
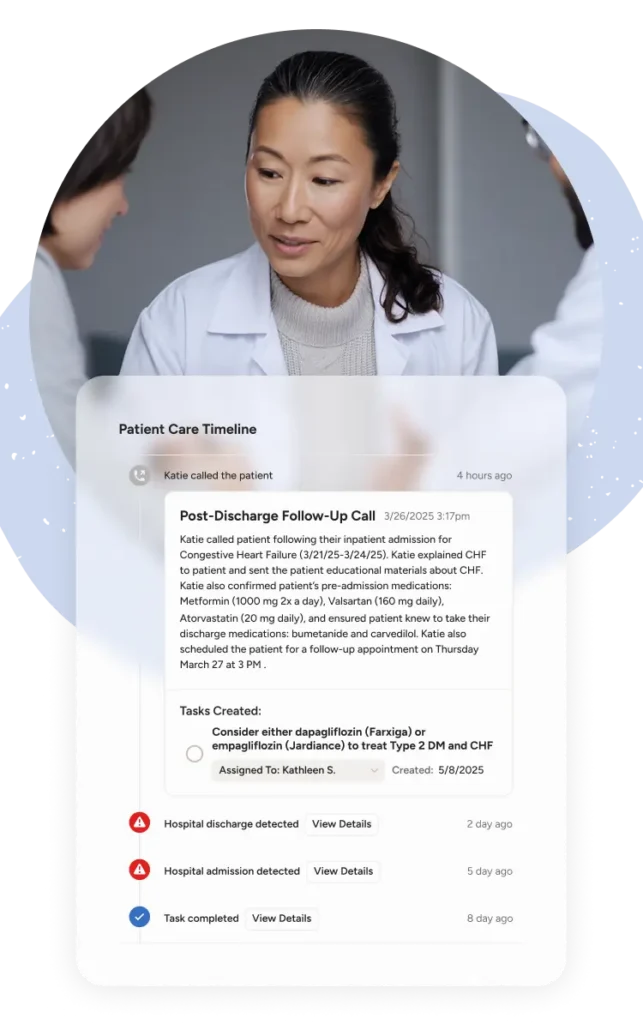
Primary care that works with physicians, not around them.
Founded at the point of care—not a boardroom—Lumeris combines physician-led insight with advanced AI to make primary care more connected, proactive, and sustainable. We partner side-by-side with health systems, physician groups, and payers to navigate complexity, accelerate performance, and deliver measurable results that last.
Lumeris is proven in practice, powered by partnership.
15+
Years of proven results
1.2M+
Lives on platform
Operational partnership
$55B
In claims ingested
Physician-first DNA
Real stories. Real transformation.
- Lumeris • December 15, 2025
Building Trust in AI: The Foundation for Adoption in Healthcare
We explored how AI in healthcare is evolving from assistive tools to…
- Lumeris • December 1, 2025
Scaling Care for the Rising-Risk Population: How Agentic AI Expands the Reach of Primary Care
Across the healthcare landscape, one truth has become impossible to ignore: there…