We’ve reached another turning point in a year of crisis and innovation. The ranks of those vaccinated and immune against COVID-19 are growing. As a nation, we’re looking forward—and asking, what comes next? The question is especially acute in healthcare as we emerge from the pandemic.
Are we, at long last, ready to leave the fee-for-service business model behind?
While long recognized as unsustainable, fee-for-service (FFS) healthcare has been persistently intransient. The pandemic, however, provides undeniable proof that volume-based systems cannot survive the disruption of a public health crisis. Doubling down on FFS is not a path forward toward sustainability. For hospitals and health systems, what comes next is an unprecedented opportunity to accelerate the shift to value.
Change is here.
That opportunity, however, will not last long. As the country begins to emerge from the crisis, disruption is swiftly becoming transformation. The outsiders have arrived to fill in gaps where traditional healthcare fell short in providing easy, remote access to healthcare. It’s no surprise that Amazon suddenly launched its primary and urgent care telehealth service. Or that CVS Health’s virtual care service, E-Clinic, is already up and running. The pandemic moved digital health, from telehealth visits to remote monitoring and hospital-at-home care, from the margins to the mainstream.
Consumers were also transformed by the crisis. They now expect healthcare to join their other services and products in providing a modernized experience. Easy points of access from digital front doors to retail care and a seamless flow of information across the patient journey are now table stakes. The inequities in their lives that drive health disparities also came into sharp focus over the past year. Addressing social determinants of health and reducing the burden of chronic conditions in lives and the economy now has broad and urgent attention.
These evolutions in care delivery, consumer expectations, and population health management are incompatible with the fee-for-service business model. We’re now at a point when recapturing your share of elective surgeries won’t restore stability. As the pandemic recedes, we must rebuild healthcare on a new foundation that ensures easy, flexible access to care that is patient-centered, addresses health disparities, and prevents and controls chronic conditions. Recovering from the pandemic and growing requires value-based care models.
Speed is of the essence.
Change in healthcare has accelerated at a pace few predicted before the pandemic. The opportunity to adapt to this new environment will be brief. Your competitors, both traditional and disruptive, are moving fast. The consolidation trend is strengthening. Risk contracting is accelerating as payers respond to the changing consumer landscape by investing in virtual, retail, and home-based care. Across the ecosystem, access to care, the social drivers of poor health, and behavioral health are rising as priorities. These urgent needs were made even more urgent during the crisis and will be critical as we face the ramifications of consumers skipping and deferring routine preventive care throughout the pandemic.
Taking decisive action now in each of these areas will determine a health system’s ability to survive—and thrive in years to come.
Hospitals and health systems can lead in this fundamentally altered environment with an agile, holistic strategy that creates resiliency and leads to growth. Now is the moment to make a resolute move to a value-based business model while maintaining financial stability in the fading days of volume-based healthcare.
Your game plan.
In the near term, before population-level immunity to COVID-19 is reached, health systems must manage capacity and staff resiliency through any surges still to come. Financials can be stabilized by recovering volume through diversified points of care. As 2022 approaches, systems must be in place that respond to new consumer behaviors and preferences and that address health equity.
To meet those challenges, move forward in three parallel avenues:
- Keep care within your system by optimizing in-network utilization
- Perform on today’s contracts by aligning operational capabilities
- Build the contracts of tomorrow to set the stage for future expansion
Concurrent progress toward these three goals will position your organization to thrive as a resilient value-based organization in a still unpredictable future. Here’s how:
Keep care within your system.
Maintaining and growing volume in your network will enable financial stability as you shift to value. To retain members and patients, begin with your physicians. A physician-led network centered on primary care will ultimately enable a better patient experience and outcomes to retain members and lower the total cost of care. True population health management is driven by physician-patient relationships supported by coordination and referral management, as well as data insights, built into the workflow. Improving in-network care delivery can translate to generating significant shared savings and increased net patient revenue for clinically integrated networks. Success requires physician and clinical team engagement, alignment and accountability, ongoing communication, and effective governance.
Perform on today’s contracts.
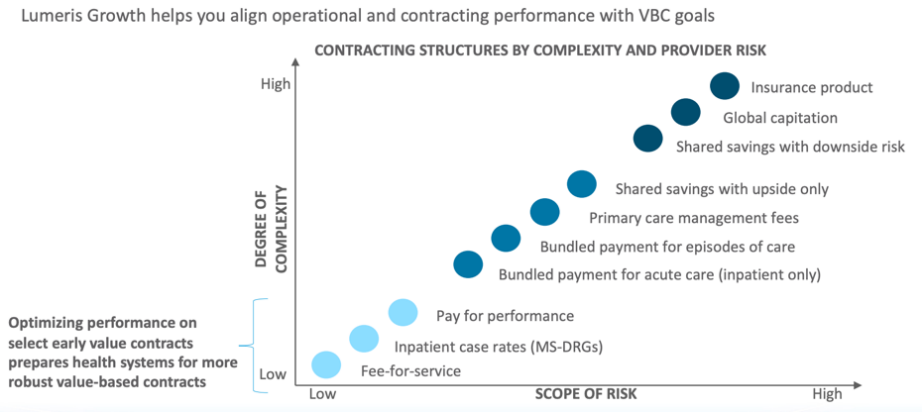
Optimize performance on your current and early value contracts to prepare your organization for more robust value-based contracts down the road. To execute on those contracts, close gaps in care and meet quality metrics with centralized management and targeted campaigns. Overall, all contracts must align with operational performance toward value-based care goals. Invest in capabilities to analyze, track, and generate dashboards for quality measures, cost, and utilization metrics, and measure progress against performance goals using claims-based data as well as pod- and physician-level data.
Build the contracts of tomorrow.
As you optimize current contracts, begin to implement a coordinated payer strategy that will evolve future value-based contracts. A comprehensive contracting strategy can help accelerate the work to diversify revenue sources and take on more risk so that you can control and lower the total cost of care. Overall, a comprehensive contracting strategy must increase your total portfolio of patient lives under these total-cost arrangements.
The path to value is challenging for every provider organization, especially on the heels of a crisis of the magnitude of the COVID-19 pandemic. And yet, given the uncertain times we face, the urgency to innovate in order to survive both the pandemic and transformation to value-based care creates an unprecedented opportunity for health systems. Now is the time to become a next-generation health system with a sustainable future.

