Our Approach
With a deep understanding of value-based care, based on more than a decade of experience, Lumeris serves as a risk-sharing operating partner to healthcare providers across the country. We provide proven clinical workflows, multi-payer contracting expertise, and comprehensive technology-powered solutions.
Clinically Led Care Transformation
Lumeris has pioneered value-based care transformation to address the total cost of care for health systems and provider groups. We deliver high quality care, while reducing costs, by focusing on what we have identified as the 6 key drivers of performance in value-based care.
These drivers represent integrated processes and proven methodologies that drive improved clinical and financial outcomes.
6 Key Drivers of Performance
in Value-Based Care
- ENTERPRISE MIND SHARE
- ALIGNED PAYER CONTRACTING
- FUNDS FLOW & PHYSICIAN INCENTIVES
- GOVERNANCE & ORGANIZATIONAL STRUCTURE
- INFORMATION, DATA & ANALYTICS
- PRACTICE TRANSFORMATION & ACCOUNTABLE CARE DELIVERY
MANAGING ALL VALUE-BASED POPULATIONS
The Right Program
for the Right Population
Across all lines of business, Lumeris has options to help you care for all patients, driving clinical, operational, and financial performance.

COMMERCIAL
PAYERS
Our partners reduce the administrative burden of balancing value-based and fee-for-service commercial contracts while maximizing performance through better network utilization of high-value providers and facilities.
MEDICAID
Our partners deploy our predictive analytics and patient engagement tools to maximize performance and improve quality outcomes and gaps in care closure for patients with the greatest SDoH risk.
TRADITIONAL
MEDICARE
Our partners participate in programs such as the Medicare Shared Savings Program (MSSP) and ACO REACH or a curated combination of both with targeted clinical support to overcome common barriers associated with the Medicare population.
MEDICARE
ADVANTAGE
Our partners participate in risk-based Medicare Advantage arrangements through our Accountable Risk Organization, a joint risk-sharing entity, which leverages our collaborative payer relationships and deep expertise in managing value-based populations and payer contracting.
OUR SOLUTION PLATFORM
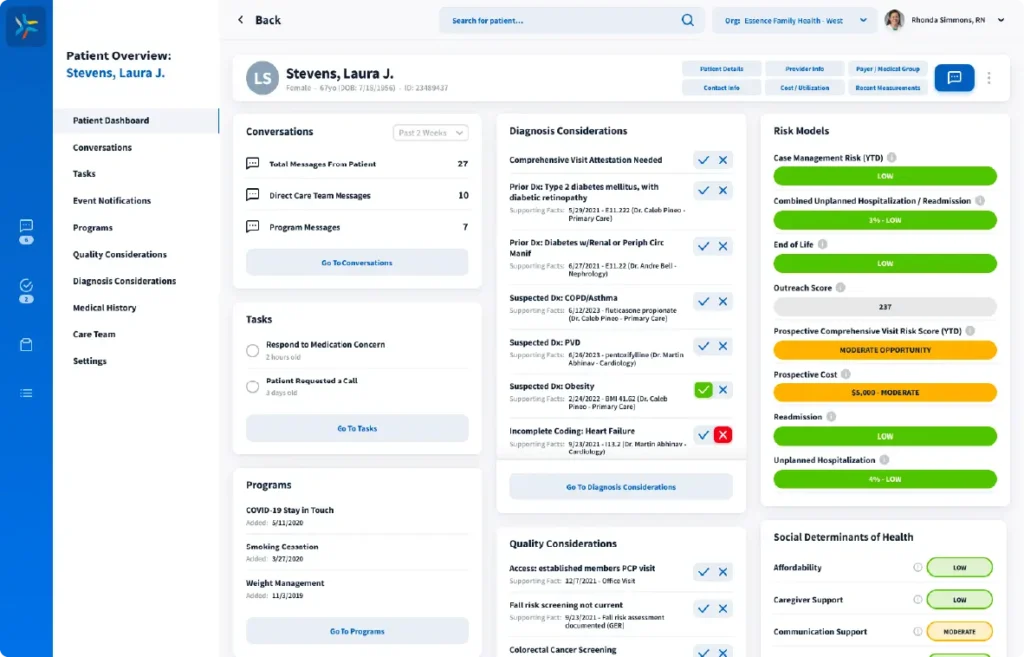
Comprehensive Value-Based Care Solution Platform to Support All Patient Lives
LumerisPerformTM is our end-to-end, Al-powered, value-based care platform made up of solutions that work together to improve patient care, lower costs, and increase savings in total cost of care risk arrangements.