The statements contained in this analysis are solely those of the authors and do not necessarily reflect the views or policies of CMS. The authors assume responsibility for the accuracy and completeness of the information contained in this document.
As the CMMI (Center for Medicare & Medicaid Innovation) Direct Contracting Program transitions to the ACO REACH Model in PY2023, it is helpful to reflect on best practice strategies for communication and alignment across stakeholders and provider networks. This is particularly relevant in advance of the August 4 provider submission deadline and the need to align stakeholders and providers around the operational mechanics of the ACO REACH Model and the activities required for success.
The following addresses lessons learned under the Direct Contracting Model and recommended areas of focus regarding communication across stakeholders prior to PY2023. The following analysis* may be most relevant for new ACO REACH administrators and providers or physician leadership entering the model for the first time in PY2023 under the Primary Care Capitation track.
Key Stakeholders to Engage
Beneficiaries: The Medicare beneficiaries who are aligned to the ACO under the ACO REACH Model either through claims-based alignment or voluntary alignment.
Providers/Physicians:
- Participating Providers (Primary Care Physicians): Participating Primary Care Physicians are the primary drivers of performance. Fundamentally, the ACO REACH Model is intended to incentivize and advance primary care coordination and it is critical for Participating Primary Care Physicians to understand the operational mechanics and what is required for success under the model.
- Participating Providers (Specialists): While certain Participating Specialists contribute to beneficiary attribution and are considered “Participating Providers” under the Model, they are not subject to primary care capitation or FFS reduction on primary care claims.
- Preferred Providers: Preferred Providers can be the remaining physician network, ancillary services, post-acute, or hospitals and support success under the Model by engaging in care management improvement activities in coordination with Participating Providers.
Practice Administrators & Staff: Often tasked with implementing the operational components of the model and the first to receive questions from providers and beneficiaries.
Group/Network Leadership: Executive leadership of the provider group or clinically integrated network – includes physician leadership and are often the champions of value-based initiatives and drivers of population health momentum within the organization.
Key Educational & Communication Topics
Network Design: The first step to entering the ACO REACH Model is finalizing the network of Participating and Preferred Providers (which must be submitted to CMS by August 4, 2022, for PY2023). However, thoughtful consideration should be given to network design as there are multiple goals that can be considered in building the network – which do not always move in sync:

Potential Network Goals
- Maximize Number of Beneficiaries (identify providers with strong Medicare FFS patient panels that are likely to be aligned under the Model’s alignment methodology)
- Maximize Performance (identify providers that have advanced on the journey of value-based care and demonstrated commitment to drive improved care coordination and primary care management)
- Promote Health Equity (identify providers in historically underserved communities with a commitment to community engagement and active outreach to underserved beneficiaries)
- Maximize Primary Care Engagement (determine whether to identify only primary care providers or include specialists as well)
- Maximize Network Growth (leverage ACO REACH to expand clinically integrated network growth across regional providers and develop network sufficiency across multiple products)
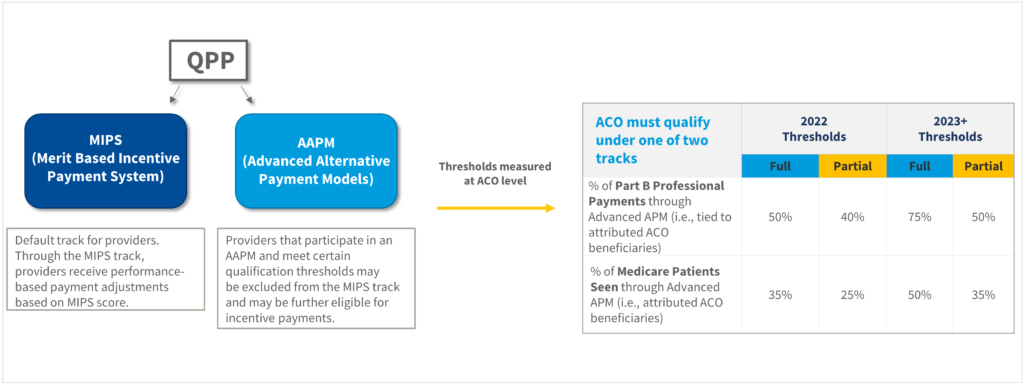
- Qualify under the Advanced Alternative Payment Model (AAPM) Threshold: (identify providers that satisfy the AAPM qualification thresholds)
ACOs will need to consider which goals are most important in coordination with their providers, acknowledging that maximizing one goal potentially impacts others. The key is to find the right network balance, considering the interests of both the ACO, providers and beneficiaries.
Benchmark & Capitation Methodology
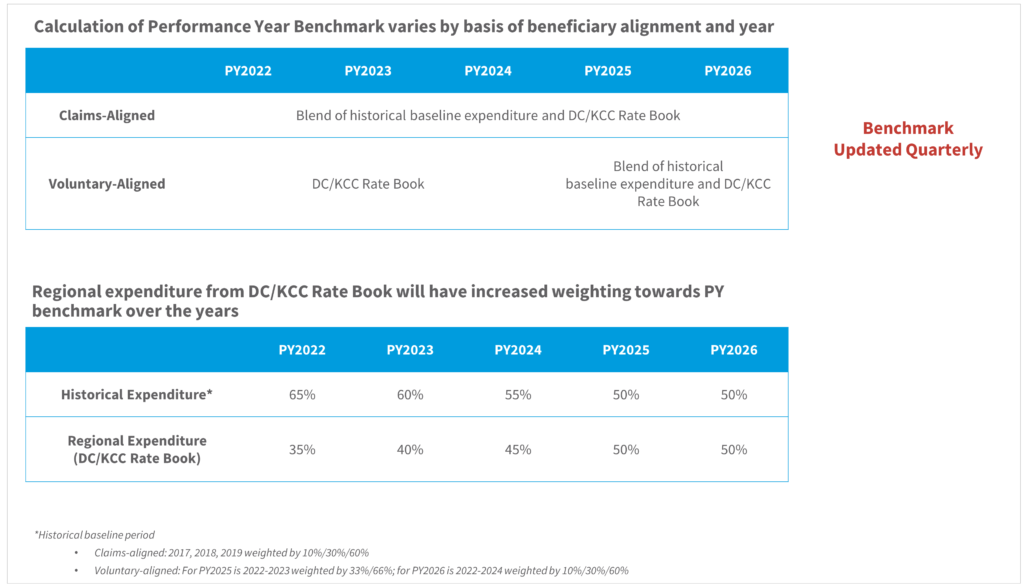
For network leadership and for certain physicians who wish to understand the finer details of the program methodology, the benchmark calculation, including historical/regional blending and USPCC trend assumptions, is an education topic worth sharing.
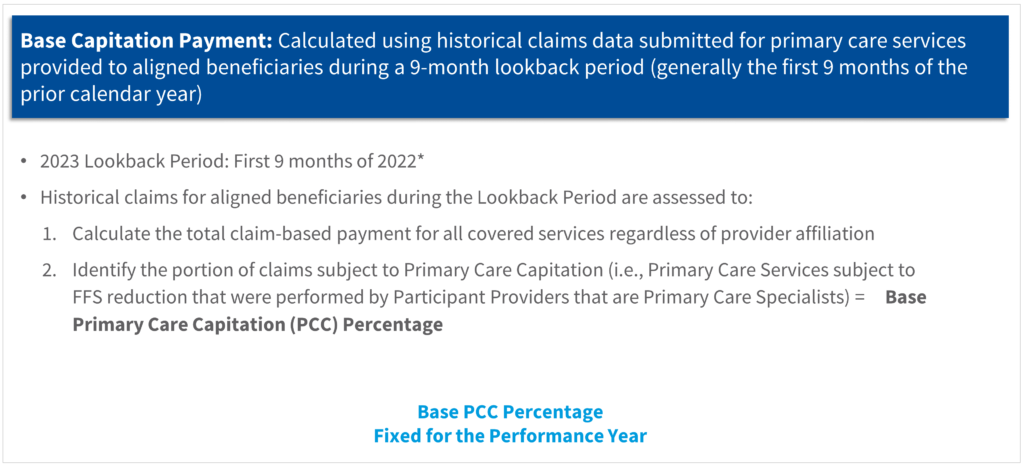
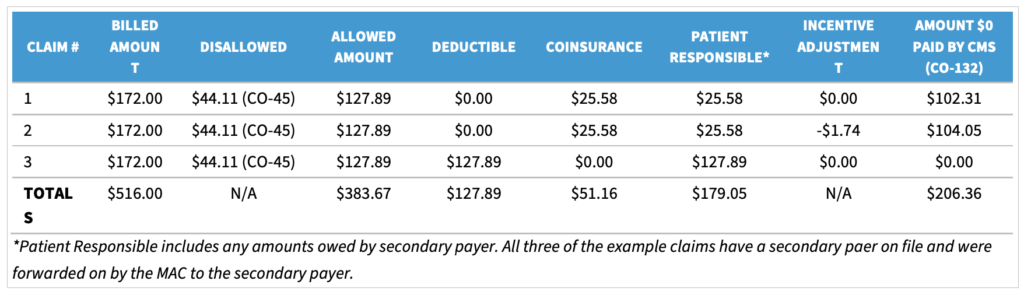
Participating Providers who have FFS payments for primary care services reduced may find it important to understand the methodology for how the corresponding capitation payment is calculated. The example below reviews the lookback period and primary care capitation proportionality calculation.
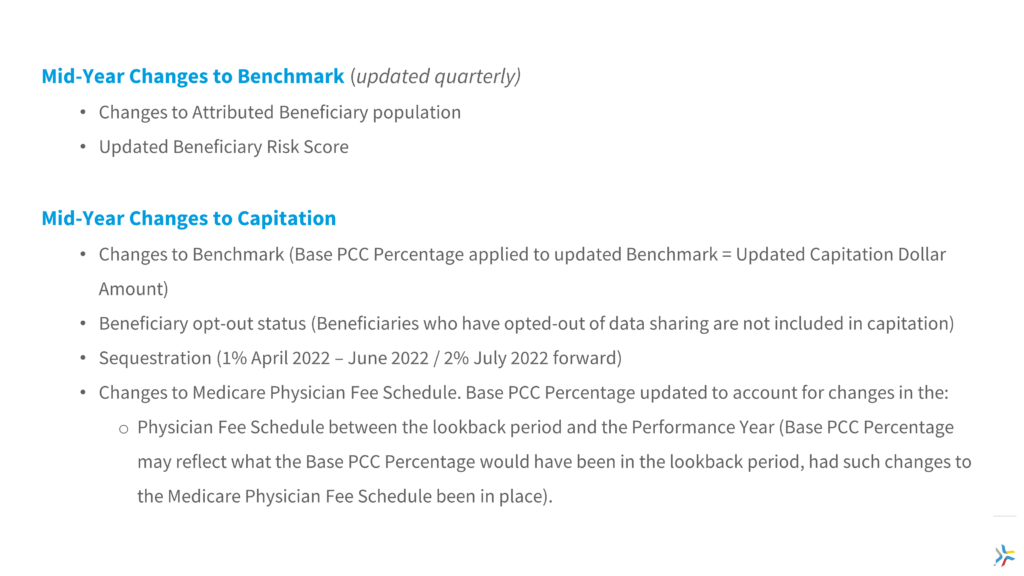
For Participating Providers and network leadership, it is important to understand the factors that can trigger mid-year adjustments to the benchmark or capitation amount, including risk score, beneficiary mix, sequestration, retrospective trend adjustments and the Physician FFS Schedule.
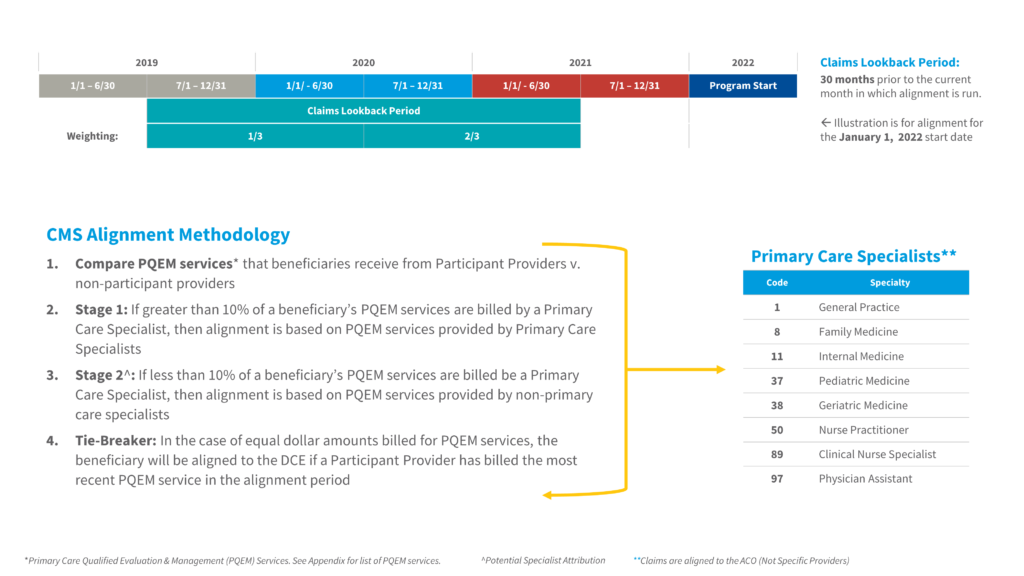
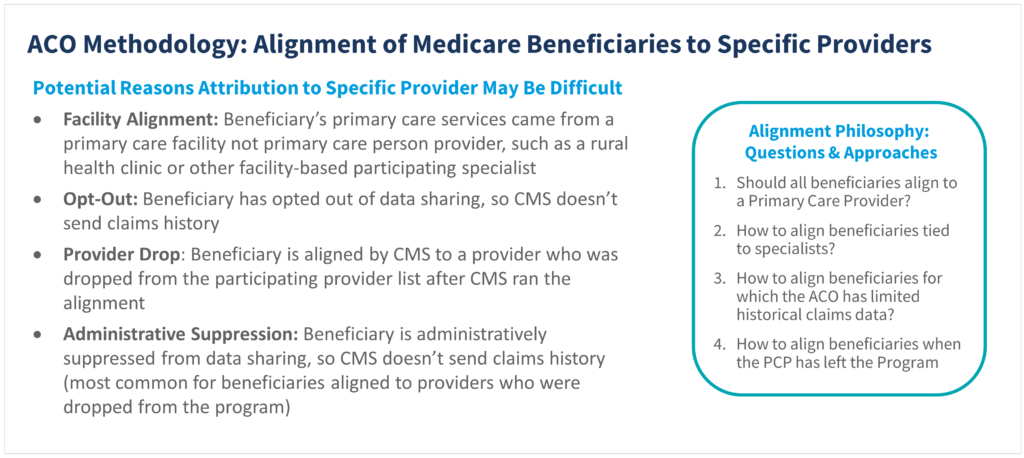
Providers, practice administrators, and network leadership will also find it beneficial to understand the ACO REACH attribution methodologies and potential challenges regarding the alignment of beneficiaries to individual providers.
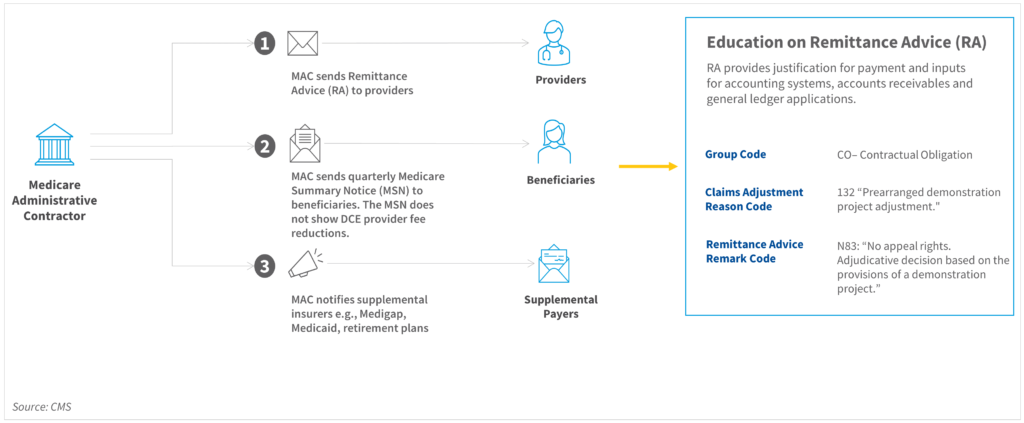
We found it important for group administration, network leadership, and providers to understand the ACO REACH Model payment mechanics, including CMS Remittance Advice Codes (CO-132). CMS has identified this as an area of undereducation for providers and has recently reminded ACOs of their responsibilities to educate providers on this topic.
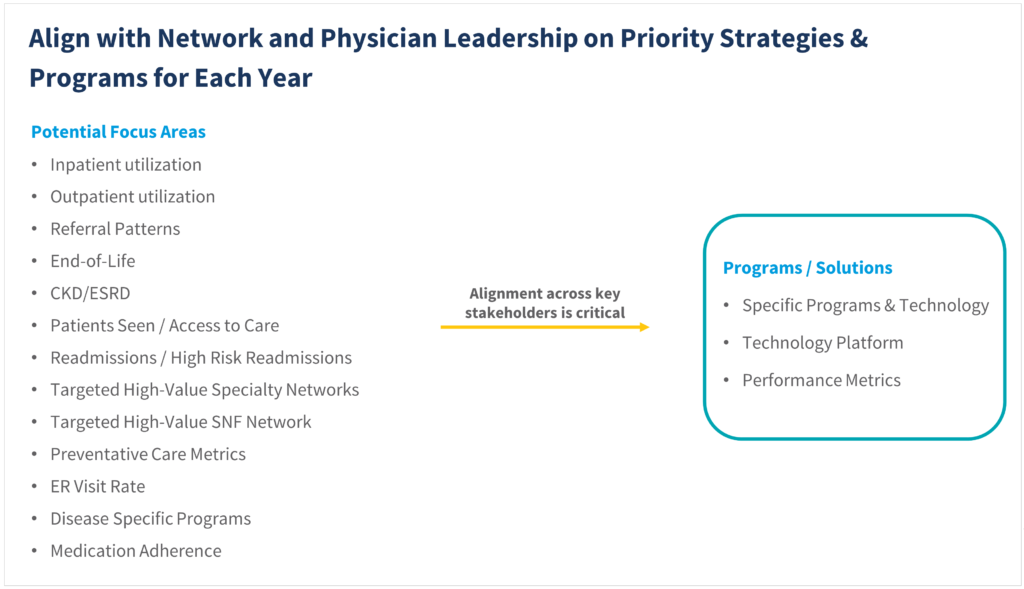
Lumeris has found it particularly important to align network and physician leadership on VBC priority strategies, programs and technology integration opportunities regarding the key areas of focus and care coordination programs. The alignment between ACOs and providers is critical to avoid change fatigue and focus on the areas of greatest opportunity for improved engagement and care coordination.
Although the Quality Payment Program (QPP) via the MACRA legislation of 2015 has been around for some time, we found that providers and network leadership appreciate education on QPP eligibility for qualified provider status under the Advanced Alternative Payment Model or AAPM qualification thresholds. Importantly, the AAPM thresholds are measured at the ACO level across the aggregate network of Participating Providers.