Joseph Satorius
Senior Vice President, ACO Programs & Strategic Operations, Lumeris
Rick Goddard
Vice President, Commercialization & Strategy, Lumeris
On February 24, CMS announced the continuation of the Direct Contracting (DC) Program under a rebranded name called the ACO REACH Model* along with several important programmatic updates. The updates primarily focus on the promotion of health equity, adjustments to benchmark and risk score methodologies, and ACO requirements to encourage greater governance engagement from participating providers. All changes take effect in 2023 and the existing DC Program remains unchanged for the remainder of 2022.
Overall, the ACO REACH modifications are positive and advance the program in ways that will benefit providers and the populations they serve. We discuss each of these changes in greater detail below along with context regarding overall impact – what’s the same, what’s different, and why that matters to your organization. Notably, CMS has improved several existing features to encourage participation in the program and has gone further to address health equity beyond any Medicare program to date.
*REACH = Realizing Equity, Access and Community Health
ACO REACH Modifications: Overview
Health Equity: Increased focus on the promotion of health equity and addressing social barriers to better help close gaps in care.
- Benchmark Adjustment: The ACO REACH Model adds a benchmark adjustment designed to reward providers with a greater proportion of historically underserved beneficiaries. Each beneficiary in the ACO Reach Model will receive a score based on the Area Deprivation Index* and dual-eligible status. The Area Deprivation Index is measured as a percentile (0-99) for each beneficiary with an additional 25 points for dual-eligible status. Using this score, CMS will stratify all aligned beneficiaries in the ACO REACH Model and the top decile will receive an upward $30 PBPM adjustment and the bottom five deciles will receive a downward $6 PBPM adjustment. The benchmark adjustment will be finalized after the Performance Year and will be applied at Final Financial Settlement.
* https://www.neighborhoodatlas.medicine.wisc.edu/ - Demographic Data Collection: ACOs must collect and report certain demographic and social determinants of health data for aligned beneficiaries. For PY2023, CMS will apply a 10% bonus to the quality withhold (not to exceed 100%) for accurately and compliantly reporting demographic data. CMS will provide additional details on this requirement prior to PY2023.
- Nurse Practitioner Benefit Enhancement: A new Benefit Enhancement will be offered to help reduce barriers to care access, particularly for beneficiaries in areas with limited access to physicians. Under this Benefit Enhancement, Nurse Practitioners will be able to assume certain responsibilities or furnish certain services without physician supervision such as certifying the need for diabetic shoes or hospice care.
Financial Methodology Updates:
- Global Discount Reduction: The benchmark discount under the Global risk-sharing option has been reduced to 3% for PY2024 (previously 4%) and to 3.5% for PY2025 and PY2026 (previously 5%).
- Quality Withhold: The Quality Withhold has been reduced from 5% to 2% of benchmark in PY2023 – PY2026.
- Benchmark Blending: The weighting of regional expenditures relative to beneficiary-specific historical expenditures in the calculation of the benchmark has been increased for PY2023 (40% vs. 35%), PY2024 (45% vs. 40%), and PY2025 (50% vs. 45%).
- Risk Score: The DC Program employs two primary approaches for deterring coding intensity: (1) an up/down 3% annual cap on risk score growth relative to a rolling reference year, and (2) application of a coding intensity factor (applied as a multiplier) to preserve a budget neutral application and limit risk score growth relative to the DC National Reference Population. While the ACO REACH Model preserves both approaches, the following updates have been made to the 3% cap on risk score growth:
- Risk score growth in PY2024 – PY2026 will be capped at 3% relative to a statice 2022 reference year (as opposed to annual 3% cap relative to rolling reference years); and
- The demographic component of the Risk Score will be factored into the 3% cap (e.g., if the demographic risk score growth from the reference year is +1%, the risk score cap would be increased to 4% upside/2% downside)
- Stop-Loss Program: The attachment points under the CMS Stop-Loss Program will be risk-adjusted to reflect beneficiary-specific risk scores and benchmarks (as opposed to a fixed attachment point under the current model).
Governance Updates: New guardrails to ensure that ACOs have meaningful governance representation and engagement from participating providers.
- Participant Provider Representation: Participating Providers or their representatives must hold at least 75% of ACO governing board voting rights (increased from 25% under the current model).
- Beneficiary Representation and Consumer Advocate: ACO governing boards must include both a Medicare Beneficiary and Consumer Advocate and these roles may no longer be held by the same individual. Both positions must have voting rights and be free from financial interest with the ACO or a Participating or Preferred Provider.
Impact of Modifications
What do those changes mean to your organization? The following summarizes the impact of the ACO REACH Model updates, which we view as generally positive for providers considering participation in the Model:
Health Equity: The ACO REACH Model supports the CMS goal of advancing health equity and improving access to care for historically underserved beneficiaries. The benchmark adjustment is intended to appropriately adjust the benchmark for beneficiaries who have historically underutilized care and encourage providers to actively engage underserved communities. The demographic data collection requirement further serves to incentivize the tracking and monitoring of social determinants and access disparities and set the expectation that health equity data and analysis should be an important component of every ACO’s care model in the same way many ACO’s track key clinical and utilization measures. Finally, CMS has provided the Nurse Practitioner Benefit Enhancement as an additional tool (along with the existing Benefit Enhancements) to reduce barriers to care and deliver improved care coordination to historically underserved beneficiaries.
The ACO Reach Model provides the tools and methodologies necessary to succeed in bringing much needed value-based strategies to historically underserved beneficiaries. Providers already engaged in or looking to expand population health and care delivery models to historically underserved communities now have a supportive value-based model and the potential to improve brand loyalty across these communities through better care deliver and improved access, particularly on a first to market competitive advantage.
Financial Methodology: The reduced discount rates for global track participants will improve the financial model for interested applicants and make it easier for smaller organizations to join the program; and the reduction of the quality withhold to 2% reduces overall performance risk by reducing the risk tied solely to achievement of defined quality metrics. In addition, the increased weighting of regional expenditures in the benchmark calculation for PY2023 – PY2025 better reward those ACOs that have historically invested in value-based care and achieved improved health outcomes relative to their geographic region. Finally, we expect the risk adjustment change (3% cap in PY2024 – PY2026 relative to a static 2022 reference year) to have a minor impact on an entity’s credit for the true acuity of the population, although the range of impact will ultimately be local provider-specific.
Overall, the financial methodology updates provide greater incentive for new participants to enter the program and more appropriately reward ACOs for historical investments in value-based care and historical delivery of improved health outcomes for the beneficiaries they serve.
Governance: The governance changes are designed to keep physicians and clinical decision-making at the forefront, similar to the Medicare Shared Savings Program. We view these changes as positive and non-problematic for ACOs with significant provider leadership and participation.
ACO REACH Eligibility for Existing DCEs: Current Direct Contracting Entities will continue in the program if they satisfy the updated governance requirements and demonstrate a strong compliance record. In addition, the model reopens a “closed” market to new applications from qualifying entities, including health systems that wish to apply independently.
Monitoring and Compliance: Organizations will be monitored for noncompliance with prohibitions against anti-competitive behavior, coding practices, and misuse of beneficiary data. Data analytics will be used to a greater extent to track the use of services over time and, compared to the population served, to assess any changes in beneficiaries’ access to care.
ACO REACH Model – Are You Ready?
Critical elements of successful value-based care model adoption through the ACO REACH Model include network design, actuarial analytics, and a unique payment distribution approach to support paying downstream providers. As with all value-based care programs, organizational alignment, engaging consumers, health equity planning deployment, open access medical cost management, care continuity, performance analytics and management, incentive design, provider engagement, and point of care solutions will also be central to your success.
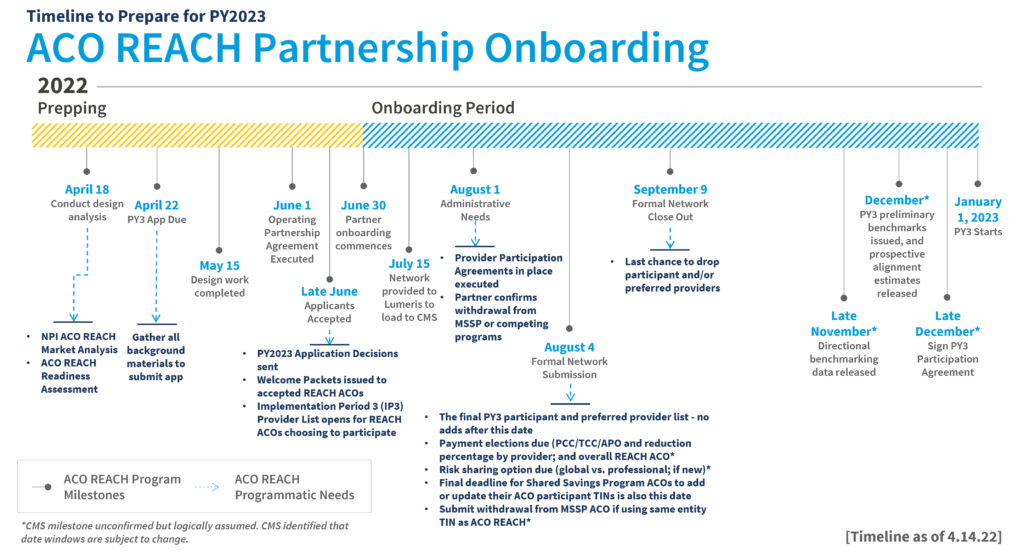
At Lumeris, we see both the importance and the impact value-based care has on communities. The new ACO REACH Model will be a key driver in the continued adoption of value-based care, and Lumeris will continue to lead the charge in empowering health systems and providers to succeed in providing the best care for their communities. As we approach the April 22 application deadline, we are prepared to assist health systems evaluate and strategize their transitions to the new ACO REACH Model. We understand what is needed to prepare and operate successfully under ever-evolving risk-based value-based care models. Likewise, we can further facilitate direct access to the ACO REACH Model for those entities that may not want to independently apply.
Have more questions or want to discuss how we can support you? Contact the Lumeris team at info@lumeris.com.

